Basic Facts:
Approximately one in eight women will be diagnosed with breast cancer in her lifetime.
Annual mammograms are recommended for women 40 and older and for younger women with specific breast cancer risk factors.
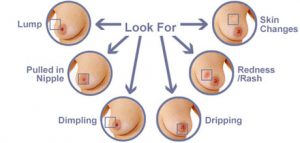
Warning signs and symptoms for breast cancer can vary greatly. If you experience any changes in the breast, nipple or underarm, schedule an appointment with your doctor.
The most common genes associated with breast cancer risk are BRCA1 and BRCA2.
There is a 98% survival rate for breast cancer that is detected at an early stage.
How Is Breast Cancer Diagnosed?
It is important to remember that a lump or other changes in the breast, or an abnormal area seen on a mammogram, may be caused by cancer or, more often, by other, less serious problems.
To determine the cause of any signs or symptoms you may have, your doctor will perform a careful physical exam that includes a personal and family medical history, as well as questions about your current overall health status. An examination that includes the following will also be done:
· Palpation. Carefully feeling the lump and the tissue around it its size, its texture, and whether it moves easily. Benign lumps often feel different from cancerous ones.
· Nipple discharge examination. Fluid may be collected from spontaneous nipple discharge and then sent to the lab to look for cancer cells. Most nipple secretions are not cancer, as an injury, infection, or benign tumor may cause discharge. For women who are at high risk for breast cancer, a procedure called ductal lavage may be used. Ductal lavage is a procedure that collects cells from inside the milk ductal system the location where most breast cancers begin.
In addition to a physical examination by your doctor, imaging tests will be performed. Imaging tests may include one or more of the following:
· Diagnostic mammography. A diagnostic mammogram is an X-ray of the breast used to diagnose unusual breast changes, such as a lump, pain, nipple thickening or discharge, or a change in breast size or shape. A diagnostic mammogram is also used to look closely at changes detected on a screening mammogram. More pictures are taken for a diagnostic mammogram than for a screening mammogram. It is a basic medical tool and is part of the workup of breast changes, regardless of a woman’s age.
· Digital mammography (also called full-field digital mammography, or FFDM). A type of mammogram in which the images are electronically captured and stored on a computer rather than X-ray film. The images are viewed on a computer screen.
· Ultrasound. This test uses high-frequency sound waves, not heard by humans, to get images of body tissues. The sound waves enter the breast and bounce back. The pattern of their echoes produces a picture called a sonogram, which is displayed on a screen. This exam is often used along with mammography.
· Scintimammography. A specialized radiology procedure sometimes used to assess the breasts when other examinations have not been clear. Scintimammography, or a molecular breast scan, is a type of nuclear radiology procedure. This means that a tiny amount of a radioactive substance is used during the procedure to assist in the examination of the breasts. The radioactive substance, called a radionuclide (radiopharmaceutical or radioactive tracer), is absorbed by certain types of body tissues. The exact role of scintimammography is unclear at this time.
· Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radio frequencies, and a computer to produce detailed images of organs and structures within the body. According to the ACS, contrast-enhanced MRI of the breasts has been shown to have a high sensitivity for detecting breast cancer in women both with or without symptoms it is recommended that high-risk women begin screening mammography and screening MRI at the age of 30, unless they and their doctors agree that a different age is more appropriate.
Based on these exams, your doctor may decide that no further tests are needed and no treatment is necessary. In such cases, your doctor may want to check you regularly to watch for any changes.
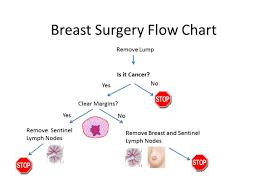
Often, however, the doctor must remove fluid or tissue from the breast to be sent to the lab to look for cancer cells. The procedure is called a biopsy. It can be done using a needle to get a piece of the area of concern, or it can be done with surgery.
A biopsy removes tissue or cells from the body for examination under a microscope. It is the only way to know for sure if cancer or other abnormal cells are present. Without a biopsy and subsequent pathology, there is no definite diagnosis.
Treatment Types:
There are many different treatments for breast cancer that involve the clinical care of a physician or other health care professional. Listed in the directory below are some, for which we have provided a brief overview.
Surgery
Post-Mastectomy
Breast Reconstruction
Lymphedema Following a Mastectomy
Post-Mastectomy Prosthesis